Cardiologists are bad for your health. This study shows that you are far more...
Cardiologists are bad for your health. This study shows that you are far more likely to survive a major cardiac event if cardiologists are out of town. Quite scary really.
Mortality and Treatment Patterns Among Patients Hospitalized With Acute Cardiovascular Conditions During Dates of National Cardiology Meetings
by Anupam B. Jena, Vinay Prasad, Dana P. Goldman, John Romley
doi:10.1001/jamainternmed.2014.6781
JAMA Intern Med. Published online December 22, 2014.
http://archinte.jamanetwork.com/article.aspx?articleid=2038979
Abstract:
Importance Thousands of physicians attend scientific meetings annually. Although hospital physician staffing and composition may be affected by meetings, patient outcomes and treatment patterns during meeting dates are unknown.
Objective
To analyze mortality and treatment differences among patients admitted with acute cardiovascular conditions during dates of national cardiology meetings compared with nonmeeting dates.
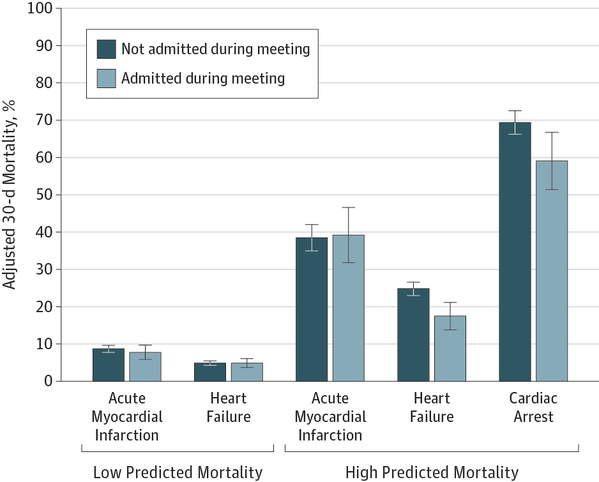
Design, Setting, and Participants Retrospective analysis of 30-day mortality among Medicare beneficiaries hospitalized with acute myocardial infarction (AMI), heart failure, or cardiac arrest from 2002 through 2011 during dates of 2 national cardiology meetings compared with identical nonmeeting days in the 3 weeks before and after conferences (AMI, 8570 hospitalizations during 82 meeting days and 57 471 during 492 nonmeeting days; heart failure, 19 282 during meeting days and 11 4591 during nonmeeting days; cardiac arrest, 1564 during meeting days and 9580 during nonmeeting days). Multivariable analyses were conducted separately for major teaching hospitals and nonteaching hospitals and for low- and high-risk patients. Differences in treatment utilization were assessed.
Exposures
Hospitalization during cardiology meeting dates.
Main Outcomes and Measures
Thirty-day mortality, procedure rates, charges, length of stay.
Results
Patient characteristics were similar between meeting and nonmeeting dates. In teaching hospitals, adjusted 30-day mortality was lower among high-risk patients with heart failure or cardiac arrest admitted during meeting vs nonmeeting dates (heart failure, 17.5% [95% CI, 13.7%-21.2%] vs 24.8% [95% CI, 22.9%-26.6%]; P
Conclusions and Relevance
High-risk patients with heart failure and cardiac arrest hospitalized in teaching hospitals had lower 30-day mortality when admitted during dates of national cardiology meetings. High-risk patients with AMI admitted to teaching hospitals during meetings were less likely to receive PCI, without any mortality effect.